I have a client who was recently admitted to the unit. Their admission assessments and associated documentation has been completed but the primary healthcare provider won't be in for another couple of hours to write medication orders. The client is complaining of moderate pain due to a headache. Can I treat this client's pain within my autonomous scope of practice (i.e., give pain medication without an order)?
What do I need to consider?
The controls on practice and the Medication practice standard can guide you in your decision-making. Your first step is to determine whether this is an activity you are:
- Authorized to perform as outlined in the
nursing regulation relevant to your designation
- Determine if there are standards, limits, and conditions you need to meet associated with the activity
- Allowed to perform in your workplace
- Competent to perform within your autonomous scope of practice
Start by thinking about the activity and the controls on practice by asking these questions:
- Does the legislation allow/restrict me from carrying out this activity?
According to the Nurses Regulation, nurses are authorized to: administer/dispense Schedule II & III medications and a limited number of Schedule I medications within their autonomous scope of practice.
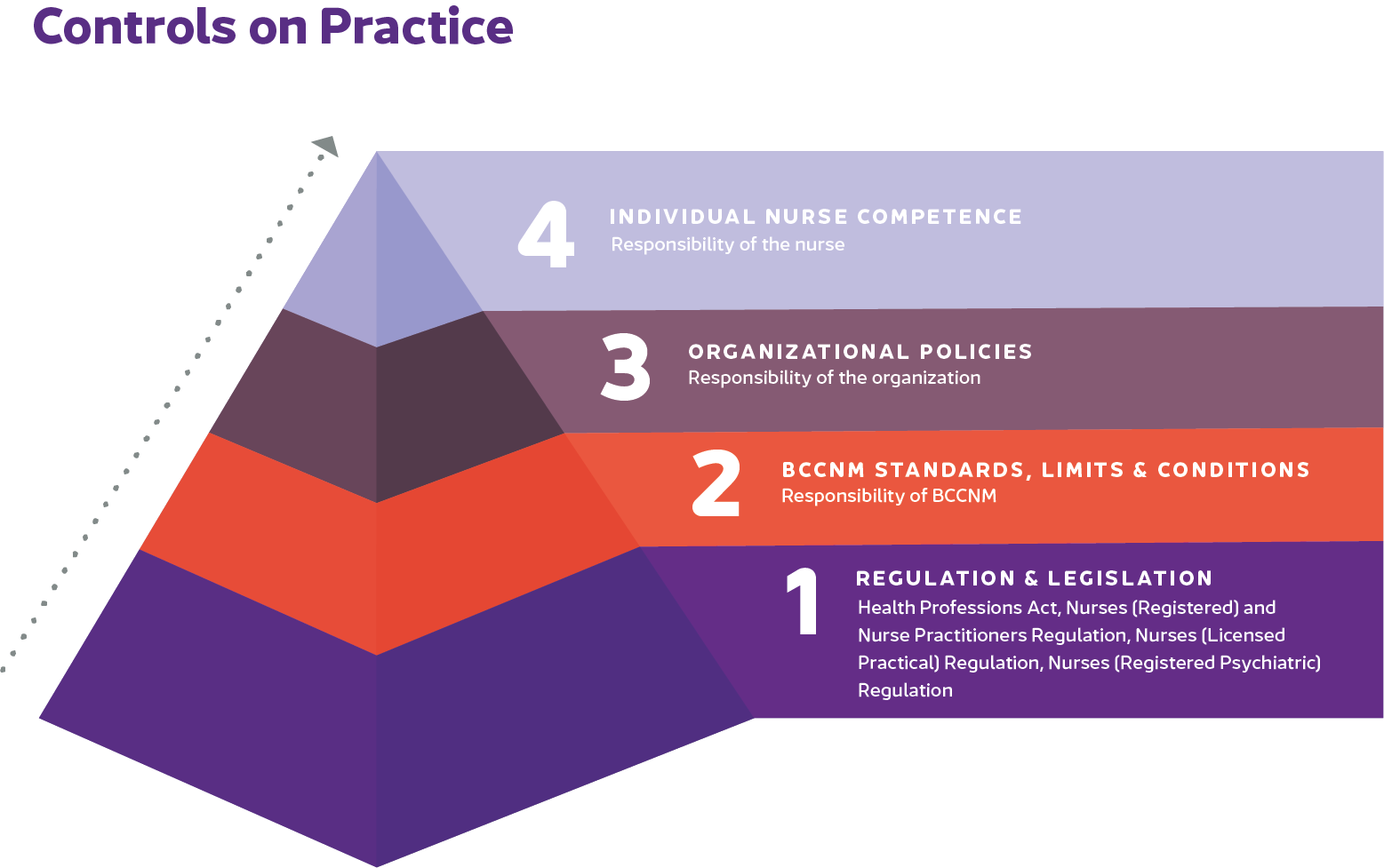
- Does BCCNM allow/restrict me from carrying out this activity?
BCCNM's standards, limits and conditions outline the requirements you need to meet when acting within autonomous scope of practice. Nurses are authorized to act within their autonomous scope of practice if they meet the principles outlined in applicable standards.
- Does my organization allow/restrict me from carrying out this activity?
Check relevant policies and protocols at your workplace for carrying out a medication-related activity without a client-specific order. Specifically, does the organization allow it? What policies need to be followed when carrying out the activity? Can you meet all these requirements?
- Does my individual competence allow/restrict me from carrying out the activity?
Evaluate your individual competence in carrying out the activity. Do you have the required knowledge, skills and abilities to do so safely?
If you determine that you are authorized to carry out the activity, review the Medication practice standard to see what additional requirements you need to meet related to medication-related activities and acting within your autonomous scope of practice. Remember, when acting within autonomous scope of practice nurses are the most accountable and responsible provider when administering or dispensing a medication without an order. Being the sole decision-maker increases risks to the client.
Additional Medication practice standard requirements:
- Following organizational policies and processes
- Assessing the client's health status including allergies
- Making or confirming a nursing diagnosis of a condition that can be improved or resolved by administering or dispensing a medication.
- Deciding if the client would benefit from the medication, considering known risks and benefits, factors specific to the client or situation, and medication alternatives
- Managing monitoring and evaluating the client's response to the medication (as applicable) including intended and unintended outcomes.
- Communicating and collaborating with the client (or their substitute decision-maker) and the health care team and document the nursing diagnosis, decision, actions, and outcomes related to the medication administered or dispensed to the client.
The
Acting within Autonomous Scope of Practice thinking tool can help you.
Decision
After reviewing the controls on practice, the Acting within Autonomous Scope of Practice standard and the Medication practice standard, you determine that you are authorized and competent to treat your client's condition within your autonomous scope of practice.
Following your workplace's protocol for autonomously treating mild to moderate pain, and consulting your client about their wishes, you administer pain medication and document your care in the client's medical record. You communicate your intervention to the client's care team.