|
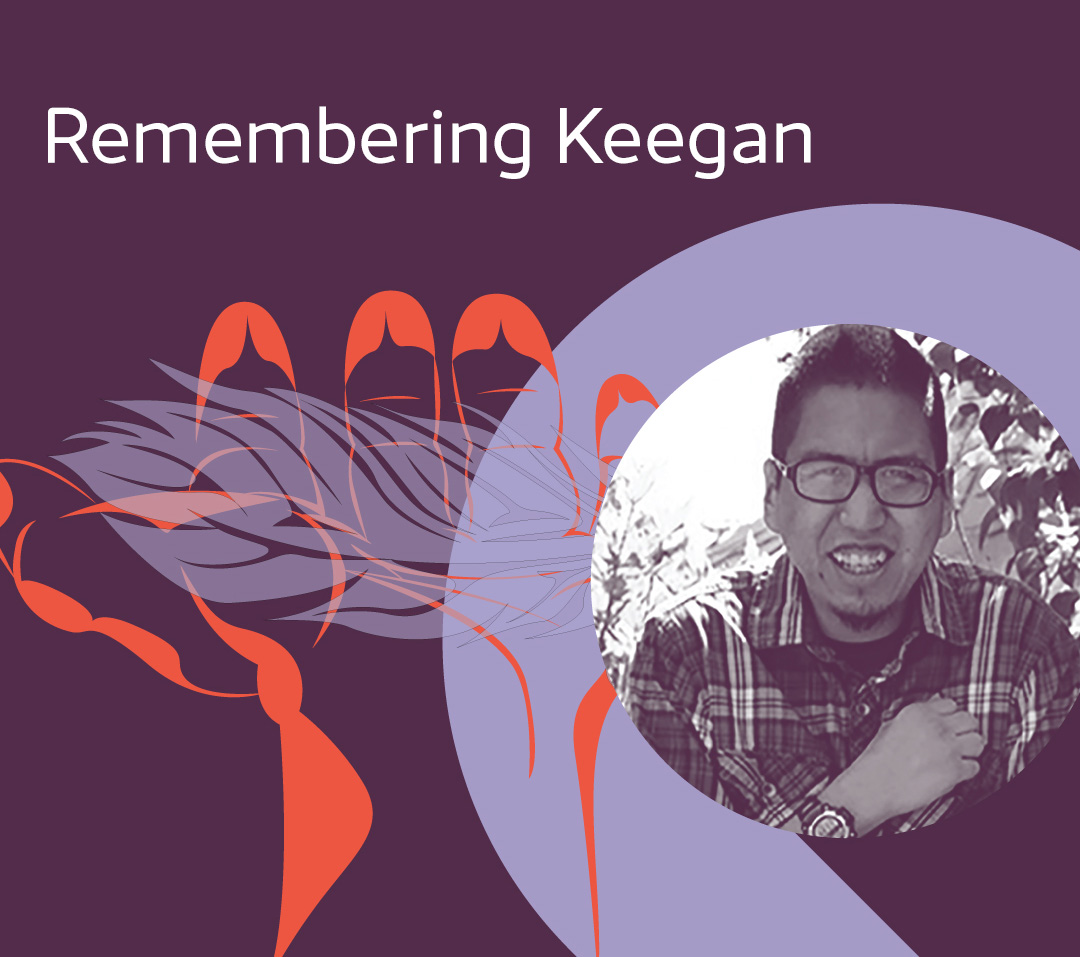 Keegan Combes — Photograph used with permission from the Keegan Combes — Photograph used with permission from the
First Nations Health Authority.
|
Keegan Combes of Skwah First Nation was a high school graduate, a grade 10 pianist and a chess champion enrolled in a trades college at the time of his death. Keegan also lived with disabilities and was non-verbal by choice.
He passed away on September 26, 2015, from a delayed diagnosis and treatment following an accidental poisoning. He was 29 years old. He is remembered, missed and loved.
Remembering Keegan: a BC First Nations Case Study Reflection was publicly released and gifted in ceremony to the B.C. health system on Keegan’s birthday, Monday, February 21, 2022.
This BC First Nations case study reflection is the first of its kind shared by BC First Nations and will help shape the Cultural Safety and quality of care for all Indigenous people in B.C. and across the country.
This Case Study Reflection is an ongoing gift from Keegan to leaders of the B.C. health system, including BCCNM. They are strongly encouraged to take the lead in the system-wide education and actions that are required to make the recommended changes.
While he is gone—he will be remembered
Keegan brought together Stó:lō and Coast Salish leaders to transform the health system from a sickness model to a wellness model of care. In Keegan's memory, the Fraser Salish Health Caucus leadership will work with the Board and Senior Executive Team of Fraser Health Authority to transform the care provided to all. In his memory, we will work together to ensure that all peoples from all places and all races will be provided the highest quality of care that is respectful of all cultures and beliefs.
Yeqwethet- Halq'eméylem
“to heal and straighten out"
We have learned through engaging with Indigenous audiences the importance of closing the loop on our learnings and that reporting back is critical to doing our work in a good way. We acknowledge with humility that we did not share our learnings or how we are implementing Keegan's Case Study Reflection and recommendations into our work on the first anniversary of receiving his gift.
Keegan's story in the news
Our commitment
- Read more about how we are honouring Keegan's legacy
-
We take this opportunity to again acknowledge the historical and ongoing harms experienced by Indigenous Peoples accessing B.C.'s health-care system and renew our commitment to helping to dismantle and eradicate Indigenous-specific racism in health care.
At BCCNM, everything we do is influenced by this commitment. We have incorporated many of the specific recommendations from the Remembering Keegan Case Study Reflection in our Redressing Harm plan, which serves as an our overarching guide towards Reconciliation. But it's more than that—it also informs our day-to-day work at the college. For example:
-
We recently surveyed our practising registrants on their uptake of our Indigenous Cultural Safety, Cultural Humility, and Anti-Racism practice standard. The practice standard came about because of our learnings from Remembering Keegan, as well as the other findings of the In Plain Sight report. We are seeing an encouraging shift—slow, but steady—in nurses' and midwives' attitudes and behaviours. They are asking for more resources to support their own learning journeys—and we're working to deliver, with a dedicated learning module planned for release later this year. This builds on the resources we created in 2022 to assist registrants in applying the standard.
-
We're on a journey as an organization, and as individuals. When setting annual professional development plans, BCCNM staff are expected to set two goals—one formal, one informal—related to increasing their knowledge and understanding of Indigenous cultural safety, cultural humility, and anti-racism.
-
We maintain a detailed dashboard of the commitments we've made in the Redressing Harm plan, including metrics, timelines, and evaluation. A core group of senior staff meet regularly to hold ourselves accountable for delivering this work, and we also keep the board closely apprised of our progress.
-
We recently introduced a Speak-up Culture framework, for staff, and are developing one for board and committee members, to create a working environment where everybody feels safe in raising concerns about behaviour they experience or witness. Nurturing a speak-up culture is a necessary step for organizations working to become anti-racist, anti-discriminatory, and anti-oppressive, and BCCNM is committed to leading this change from within. We will be sharing more in the coming months.
-
We are actively working with other B.C. health regulatory bodies to increase collaboration and share learnings and resources to reduce the impact on and potential for re-traumatizing those coming forward.
Things we are continuing to work on include:
-
Developing e-learning modules regarding the ethical use of interventions, including seclusion and restraint, which will also connect to the Indigenous Cultural Safety, Cultural Humility & Anti-Racism practice standard. This module directly addresses recommendations from Remembering Keegan.
-
Developing mandatory training for all staff, board, and committee members.
-
Improving our complaints processes from intake to outcome, by being patient, family, and community centred.
-
Developing plain language information to guide families to the bodies to provide appropriate feedback.
-
Ensuring nursing and midwifery education programs incorporate the Indigenous Cultural Safety, Cultural Humility & Anti-Racism practice standard into entry-level education.
-
Sharing learning resources, including the Remembering Keegan case study, with other health system partners.
In undertaking this important work, we continue to be guided by Elders, Knowledge Keepers, and Indigenous Peoples. And we are also guided by Keegan's truth and Case Study Reflection.
His life and legacy lives on in our commitment to eradicating Indigenous-specific racism to make the health-care system safe for Indigenous Peoples. We will know we have achieved this when Indigenous people tell us we have.
|